This is the third and final article in a series on preparation strategies for the Marathon des Sables. This article series discusses heat acclimation for runners, heat stress, the impact of heat on gut function, and the consequences for nutritional choices when exercising in the heat. In the first article we discussed various aspects of heat acclimation. In the second article we followed this with a discussion on heat acclimation specifically for women.
This final article will now cover the relationship between heat stress and gut function and provide some nutritional tips for runners taking on the Marathon des Sables. One reason I wanted to bring this topic up is that many runners are not aware of the connection between heat stress and gut function. We observed an enormous amount of gastrointestinal issues in the 2021 edition of the MDS, which was also one of the hottest on record. That should be a lesson to not ignore heat acclimation, and to consider what else you can do to minimise GI distress during the race.
I thank Drs Ash Willmott and Justin Roberts for their contributions and for taking the time to respond to my questions.
Can heat cause gastrointestinal problems for runners?
Recent research highlights that a high percentage of endurance athletes tend to suffer to some degree of gastrointestinal (GI) discomfort or distress during both training and events, particularly when exposed to heat stress (Prado de Oliveira et al., 2014). Whilst prevalence rate differs, some 30-50%+ of athletes report varying degrees and severity of GI complaints, indicating the impact of endurance exercise in heat stress on individual gut function. In fact, in one ultra-race, some 96% of runners reported some form of GI complaint (Stuempfle et al., 2015) with nausea being most commonly reported. Along with appetite suppression, acute weight loss and reduced stimulus to drink, this is one pathway that contributes to heat-related illnesses. It can compromise an individual’s thermoregulation, health, performance, and obviously the enjoyment of the event.
Specifically, the increased physiological strain (such as a high core temperature ≥39.0°C, reduced blood flow to the gut, increased cardiovascular strain and dehydration) whilst running in the heat, can negatively affect GI barrier integrity and function. This can ultimately lead to transient GI permeability compared with exercising within cooler conditions (Snipe et al., 2018; Costa et al., 2020; Walter et al., 2021).
So what happens in the body and to the gut when exercising in heat stress?
These “gut” related issues occur as athletes exercise for prolonged or intense periods in heat stress. Blood flow is redistributed away from the “gut” and towards the skeletal muscles (e.g. to continue exercising) and also towards the peripheral circulation to support heat dissipation and thermoregulation. This results in a range of negative outcomes, including:
- reduced splanchnic perfusion (or, less blood flow to the abdominal organs, including the stomach, liver, and intestines),
- gastrointestinal ischemia (or, reduced gut blood flow),
- epithelial cell injury and tight junction damage to the gut itself and,
- a “leaky gut”, where endotoxins or bacteria escape from the gut and enter blood circulation.
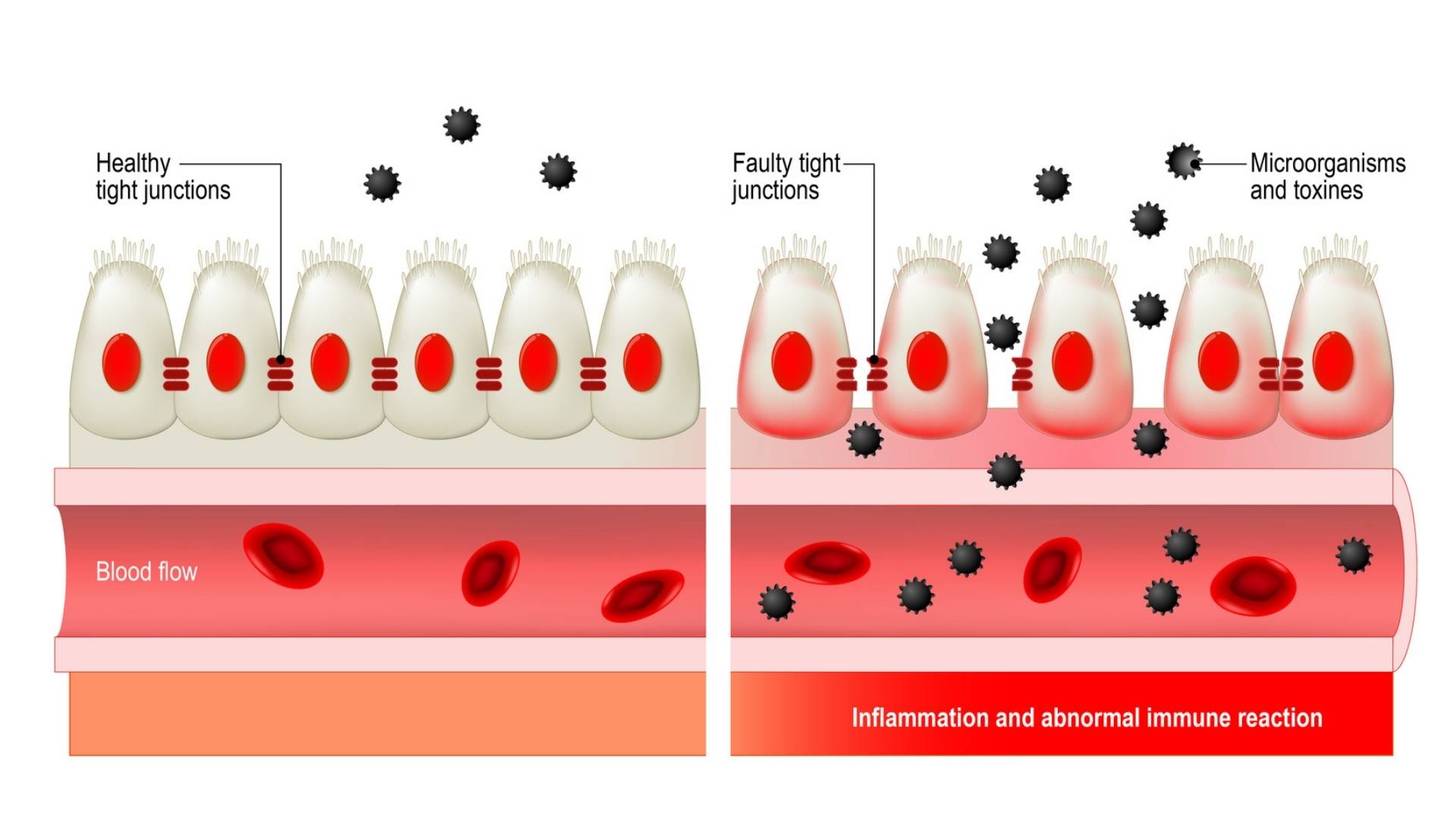
Alongside this, athletes may experience suppressed gastric (or stomach) emptying, which can lead to a range of negative symptoms, such as nausea and dizziness, upper abdominal pain, flatulence, belching and bloating and, an urge to defecate (van Wijck et al., 2011; Costa et al., 2017; Walter et al., 2021). These are things individuals don’t need when running in the dunes of the Sahara!
Disrupted GI function can affect individuals in different ways. Sometimes during acute recovery from completing a race stage (0-4 hours), or perhaps with a delayed response (4-48+ hours). Acute ‘endotoxemia’ may evoke immune and inflammatory responses, which can lead to septic shock, systemic inflammatory response syndrome and/or heat stroke, and therefore needs attention.
Women may be more vulnerable to GI symptoms
Furthermore, females may be more vulnerable to GI symptoms during exercise. This is due to hormone variations across the menstrual cycle, and, changes in visceral sensitivity (e.g. gut pain sensation) and gastrointestinal motility (e.g. movements of the digestive system). This is especially pertinent during menses (i.e., low oestrogen and progesterone) and the luteal phase of the menstrual cycle (i.e. high oestrogen and progesterone levels) (Lei et al., 2017).
Carbohydrate use increases but absorption rate decreases
Exercising in heat stress can highly modify carbohydrate (CHO) metabolism. Research suggests that CHO oxidation (carbohydrate use) increases during exercise in the heat compared with ambient temperatures. This is caused by a 25% increase in muscle glycogen use, and it results in increased blood lactate concentrations.
As mentioned earlier, heat stress reduces the blood flow to the intestine. This may impair the absorption of CHO (and other nutrients), which may lower the oxidation rate of ingested CHO by up to 10%. These factors are likely influenced by the uptake and release of consumed glucose by the liver, glucose transport to the muscle, gastric emptying, and intestinal absorption of glucose (Jentjens et al., 2002). We all have individual responses to these and so there will be individual variation.
So, although CHO use increases during exercise in the heat, there is a limitation in intestinal absorption and it’s not as simple as just ingesting more CHO. This highlights the need for heat acclimation (and also potentially gut training). A practical recommendation based on current evidence is to target 30-60g of CHO intake per hour.
How does heat impact the body’s ability to digest food?
The challenge here is the individual nature and response to exercising in the heat. Athletes report symptoms that range from ‘trivial’, mild to moderately ‘uncomfortable’ through to sustained, painful and ‘performance impairing’. Interestingly a high percentage use of non-steroidal anti-inflammatory drugs (NSAIDs) have been reported where severe symptoms have been noted (Schwartz et al., 1990).
Exercising in the heat can reduce gastric emptying rate. As core temperature increases there is a reduction in both stomach and GI ‘motility’ (movements). This can impact on active CHO transport and GI absorption rates. Basically, if you aim to maintain a strict fuelling and hydration schedule this may not work out as planned.
Multiple types of sugars
Studies have demonstrated a strategic benefit of consuming ‘multiple transportable CHO’ in the heat, such as drinks containing both glucose and fructose. This is because of higher exogenous oxidation rates (that is a high rate of carbohydrate ‘use’ from the consumed drink) and fluid availability (Jentjens et al., 2006). Based on this it is potentially beneficial to not rely on a single CHO type but to look for products that have multiple sugars. This could potentially maximise transport based on the previous limitations mentioned. Furthermore taste can change throughout a race like the Marathon des Sables, and this would be another argument for variety of food and snacks, such as both sweet and savoury options.
It is also known that dehydration (or rather ‘exercise-induced hypohydration’) goes hand in hand with GI barrier disruption. This is independent of heat stress and can further ‘aggravate’ the ability to digest/absorb key nutrients. This is another reason why heat acclimation and fluid maintenance may be vital during event preparation.
What do we know about fuelling for ultra-marathons?
On the one hand, generalised fuelling guidelines for endurance and ultra-endurance events recommend upwards of 30-60 g of CHO delivery per hour and 400-800 mL of fluid delivery per hour. Indeed, there is evidence that race finishers tend to consume higher amounts of total CHO over single stage ultra-marathons (~1g/kg/hr of CHO) compared with non-finishers (~0.6g/kg/hr; Stellingwerff, 2016). However, such high ingestion rates (particularly up to 90g/hr) may be unrealistic for longer duration events (Tiller et al., 2019) and can lead to GI discomfort and distress later in the race. This can also be further problematic for multiple stage events.
On the other hand, most ultra runners do not typically rely exclusively on a sports drink/gel approach and tend to have greater preference for energy rich (fat) and savoury (sodium rich) foods. In fact, one study demonstrated that over a 100-mile race, finishers tended to consume more total fat (~98g) compared with non-finishers (~19g [Stuempfle et al., 2011]). This highlights that a degree of tolerance to both CHO and fat may be required for successful ultra-race completion (Tiller et al., 2019).
Challenges of the Marathon des Sables
However, the MDS is a completely different beast when it comes to nutrition, mainly because of the self-sufficiency required. The race organisers specify that athletes are required to carry a minimum of 2000 kcal per day, which ultimately means that the majority of your backpack is (yes you’ve guessed it)… food. The other challenge is competing with the demands of the event whilst adhering to a practical fuelling/hydration strategy. During early morning starts, the tent you are under is literally removed whilst you are snuggly tucked up, leaving you (and your race colleagues) to basically wake up and get to work on packing up for the day whilst having whatever breakfast you have prepared. Interestingly, ingestion of CHO before exercise may help to reduce potential for in-race GI permeability.

Once you start moving, checkpoints are roughly every 10 km or so. Water is rationed and the amounts handed out vary but are detailed in the race rules and the road book. The bottles have typically sat in the sun for a while so tend to be lukewarm. As a result it is a good idea to train in preparation for the event with slightly warmer water (which sounds contradictory) but that is what you will be up against.
What are your practical nutrition and equipment tips for the Marathon des Sables?
- Aim to get your backpack as light as possible (the general range is between 6-15 kg, with many runners aiming for 7-9 kg – all kit/food)
- Ask whether you are ‘racing’ or ‘aiming to finish’, this might determine what ‘luxuries’ you are prepared to carry
- Whilst the event minimum is 2000 kcal per day, aim to estimate daily intake in a spreadsheet in the weeks leading into the race. Find out where your ‘happy medium’ is (it will likely be closer to 2600-3000 kcal per day, which may be a practical trade off)
- If using expedition type food packs, consider emptying contents into a vacuum sealed pack and trim off the edges to save weight. This might sound strange, but you could save upwards of 300g, and use less packing space.
- Consider two options for breakfast, i) either high energy, CHO/fat dense foods e.g. expedition porridge or granola with creamer or milk powder (perhaps add in extra chia seeds or protein powder), or ii) have a liquid based breakfast (e.g. a CHO/electrolyte drink followed by a protein drink) if you are more susceptible to gut cramps or not overly hungry), then revert to your ‘grazing’ strategy over the day.

- If you do suffer from gut sensitivity or GI issues, be mindful of early morning fat/fibre content of your foods.
- Over the day consider general variety – i.e. a mixture of solid foods (e.g. Clif bars, shot bloks, Peperami/Jerky, trail mix) and liquid foods (e.g. added electrolytes, mixed CHO solutions (e.g. Tailwind/Xendurance/High5 Energy Source). Aim to consume and hydrate every 20-45 minutes (pending personal preference), or take a ‘drink to thirst’ approach. If doing this be mindful of total electrolytes being consumed. The race organisers provide each athlete with a set amount of salt tablets. Consuming 1-2 salt tablets per hour (~500-1000 mg) along with suitable fluid ingestion tends to negate issues associated with sodium ‘depletion’/ hyponatraemia and dehydration.
- Useful tip: take additional effervescent electrolyte tablets which can be added to the water bottles to increase drink palatability
- Be mindful that water given to you in sealed bottles may be warm (especially mid stage) and tend to be less ‘desirable’ to drink. It may be worth trialling this in training to ensure you can still meet a planned strategy. This may form part of a gut training preparation approach.
- When you finish each stage aim to maximise recovery via consumption of a protein recovery drink and a CHO rich electrolyte drink. You could, for example, use one of the bottles provided, then use that bottle as a container to consume your evening meal (by cutting it in half) and saving on weight carried.
- For evening (and breakfast meals) decide on whether you want to eat warm or cold foods. If the latter, then you will save weight by not having to carry a mini-stove. That said, many of the expedition foods don’t taste great with just cold water so it is wise to test this in training.
- For evening meals, consider variety in your approach. You can get extra CHO into these meals by adding rice or crushed noodles (which are both lightweight). Also try grazing on smaller snacks later into the evening.
Consider a multi-nutrient and amino acids
Ultimately, the foods you choose to take will be based on personal preference, weight economy, taste and ease of preparation. Effectively, over the event you will likely compromise overall dietary quality, so having a daily multi-nutrient could be a useful approach. Various nutrients are currently being explored to assess whether they have physiological and practical applications to protecting the gut during sustained exercise in the heat.
For example, specific amino acids such as glutamine and arginine may have potential ‘protective’ effects, particularly when daily dietary intake is low. This may also apply to polyphenol rich foods containing curcumin and other antioxidant nutrients (King et al., 2021). There is also interest in the use of pre and probiotic strategies which may support reduction of pre and in-race GI symptoms (Roberts et al., 2016; Pugh et al., 2017; Pugh et al., 2019). However, based on the wide variation and responses observed between athletes, further research is needed to confirm or support current findings.
Summary: Nutritional Recommendations to Support Gut Function whilst Exercising in Heat Stress
- Consider early nutrition preparation during your training build up; speak with a qualified nutrition professional to tailor requirements
- If you are sensitive to GI issues or risk of GI permeability, consider use of probiotics and/or amino acid strategies to support the gut in the lead in phase (e.g. 4-8 weeks before)
- Carefully consider event requirements and practicalities/weight of overall food
- Carefully consider food/snack and in-stage fuelling variety
- Aim to start each stage in a state of normal hydration (using cooler fluids if accessible) and consider ingesting a CHO rich breakfast, and L-glutamine two hours prior to exercising (0.25-0.9 g per kg of fat free mass) (Pugh et al., 2017)
- Target tolerable amounts of CHO across each stage (e.g. 30-60+ grams per hour of a liquid multi-transportable CHO), along with easily digestible CHO preferences (gels/shot blocks etc.), and include other more savoury snacks (jerky, trail mix) as needed
- Aim to avoid ‘overhydration’ during prolonged exercise to minimise risk of hyponatraemia (although this is unlikely during the MDS based on rationed water)
Further Reading, Contact Information, Resources & References
Here is a related article on nutritional considerations for ultra-marathon training and racing:
- Tiller NB, Roberts JD, Beasley L, Chapman S, Pinto JM, Smith L, Wiffin M, Russell M, Sparks SA, Duckworth L, O’Hara J, Sutton L, Antonio J, Willoughby DS, Tarpey MD, Smith-Ryan AE, Ormsbee MJ, Astorino TA, Kreider RB, McGinnis GR, Stout JR, Smith JW, Arent SM, Campbell BI, Bannock L. International Society of Sports Nutrition Position Stand: nutritional considerations for single-stage ultra-marathon training and racing. J Int Soc Sports Nutr. 2019 Nov 7;16(1):50.
Twitter:
Dr Ash Willmott – @AshWillmott / https://aru.ac.uk/people/ash-willmott

Dr Justin Roberts – @drjustinroberts / https://aru.ac.uk/people/justin-roberts

If you are interested in:
- Nutrition guidance for endurance and ultra-endurance events – contact Dr Justin Roberts
- Altitude exposure, information and education – contact Dr Ash Willmott or visit Para-monte.org
References
- Costa, R. J., Gaskell, S. K., McCubbin, A. J., & Snipe, R. M. (2020). Exertional-heat stress-associated gastrointestinal perturbations during Olympic sports: Management strategies for athletes preparing and competing in the 2020 Tokyo Olympic Games. Temperature, 7(1), 58-88.
- de Oliveira EP, Burini RC, Jeukendrup A. Gastrointestinal complaints during exercise: prevalence, etiology, and nutritional recommendations. Sports Med. 2014 May;44 Suppl 1(Suppl 1):S79-85.
- Jentjens RL, Underwood K, Achten J, Currell K, Mann CH, Jeukendrup AE. Exogenous carbohydrate oxidation rates are elevated after combined ingestion of glucose and fructose during exercise in the heat. J Appl Physiol (1985). 2006 Mar;100(3):807-16.
- Jentjens, R. L., Wagenmakers, A. J., & Jeukendrup, A. E. (2002). Heat stress increases muscle glycogen use but reduces the oxidation of ingested carbohydrates during exercise. Journal of applied physiology, 92(4), 1562-1572.
- King MA, Rollo I, Baker LB. Nutritional considerations to counteract gastrointestinal permeability during exertional heat stress. J Appl Physiol (1985). 2021 Jun 1;130(6):1754-1765. doi: 10.1152/japplphysiol.00072.2021. Epub 2021 May 6. PMID: 33955260.
- Ogden, H. B., Child, R. B., Fallowfield, J. L., Delves, S. K., Westwood, C. S., & Layden, J. D. (2020). The gastrointestinal exertional heat stroke paradigm: pathophysiology, assessment, severity, aetiology and nutritional countermeasures. Nutrients, 12(2), 537.
- McCubbin, A. J., Allanson, B. A., Odgers, J. N. C., Cort, M. M., Costa, R. J., Cox, G. R., … & Burke, L. M. (2020). Sports dietitians Australia position statement: nutrition for exercise in hot environments. International journal of sport nutrition and exercise metabolism, 30(1), 83-98.
- Pugh, J. N., Sage, S., Hutson, M., Doran, D. A., Fleming, S. C., Highton, J., … & Close, G. L. (2017). Glutamine supplementation reduces markers of intestinal permeability during running in the heat in a dose-dependent manner. European journal of applied physiology, 117(12), 2569-2577.
- Pugh JN, Sparks AS, Doran DA, Fleming SC, Langan-Evans C, Kirk B, Fearn R, Morton JP, Close GL. Four weeks of probiotic supplementation reduces GI symptoms during a marathon race. Eur J Appl Physiol. 2019 Jul;119(7):1491-1501. doi: 10.1007/s00421-019-04136-3.
- Roberts JD, Suckling CA, Peedle GY, Murphy JA, Dawkins TG, Roberts MG. An Exploratory Investigation of Endotoxin Levels in Novice Long Distance Triathletes, and the Effects of a Multi-Strain Probiotic/Prebiotic, Antioxidant Intervention. Nutrients. 2016 Nov 17;8(11):733. doi: 10.3390/nu8110733.
- Schwartz AE, Vanagunas A, Kamel PL. Endoscopy to evaluate gastrointestinal bleeding in marathon runners. Ann Intern Med. 1990 Oct 15;113(8):632-3.
- Stellingwerff T. Competition Nutrition Practices of Elite Ultramarathon Runners. Int J Sport Nutr Exerc Metab. 2016 Feb;26(1):93-9.
- Stuempfle KJ, Hoffman MD, Weschler LB, Rogers IR, Hew-Butler T. Race diet of finishers and non-finishers in a 100 mile (161 km) mountain footrace. J Am Coll Nutr. 2011 Dec;30(6):529-35. doi: 10.1080/07315724.2011.10719999
- Stuempfle KJ, Hoffman MD. Gastrointestinal distress is common during a 161-km ultramarathon. J Sports Sci. 2015;33(17):1814-21. doi: 10.1080/02640414.2015.1012104
- Snipe, R. M., Khoo, A., Kitic, C. M., Gibson, P. R., & Costa, R. J. (2018). The impact of exertional-heat stress on gastrointestinal integrity, gastrointestinal symptoms, systemic endotoxin and cytokine profile. European journal of applied physiology, 118(2), 389-400.
- Snipe, R. M., & Costa, R. J. (2018). Does biological sex impact intestinal epithelial injury, small intestine permeability, gastrointestinal symptoms and systemic cytokine profile in response to exertional-heat stress?. Journal of sports sciences, 36(24), 2827-2835.
- Tiller NB, Roberts JD, Beasley L, Chapman S, Pinto JM, Smith L, Wiffin M, Russell M, Sparks SA, Duckworth L, O’Hara J, Sutton L, Antonio J, Willoughby DS, Tarpey MD, Smith-Ryan AE, Ormsbee MJ, Astorino TA, Kreider RB, McGinnis GR, Stout JR, Smith JW, Arent SM, Campbell BI, Bannock L. International Society of Sports Nutrition Position Stand: nutritional considerations for single-stage ultra-marathon training and racing. J Int Soc Sports Nutr. 2019 Nov 7;16(1):50. doi: 10.1186/s12970-019-0312-9.
- Walter, E., W Watt, P., Gibson, O. R., Wilmott, A. G., Mitchell, D., Moreton, R., & Maxwell, N. S. (2021). Exercise hyperthermia induces greater changes in gastrointestinal permeability than equivalent passive hyperthermia. Physiological Reports, 9(16), e14945.
